What is Atrial Flutter?
Hello dear readers, on this platform dedicated to your heart health, today I want to explain in detail a heart rhythm disorder that I frequently encounter in my cardiology practice but is perhaps not sufficiently known to the public: atrial flutter. Your heart’s regular beats are fundamental to its efficient pumping of blood throughout your body. Even the slightest disruption in this rhythm can lead to significant health problems. Atrial flutter is one such disruption and is a condition that must be taken seriously.
Atrial Flutter vs. Atrial Fibrillation: Two Close Neighbors
Atrial flutter and atrial fibrillation (AF) are two common types of arrhythmias originating from the atria, the heart’s upper chambers. Both can cause irregular and rapid heartbeats, but there are crucial differences between them:
- Atrial Fibrillation (AF): The atria produce uncoordinated, chaotic electrical signals. This causes the atria to quiver (fibrillate) and fail to pump blood effectively. The electrical signals transmitted from the atria to the ventricles are also irregular, leading to irregular and often rapid ventricular beats. AF’s appearance on an EKG is characterized by irregular R-R intervals and irregular fibrillation waves replacing the P waves.
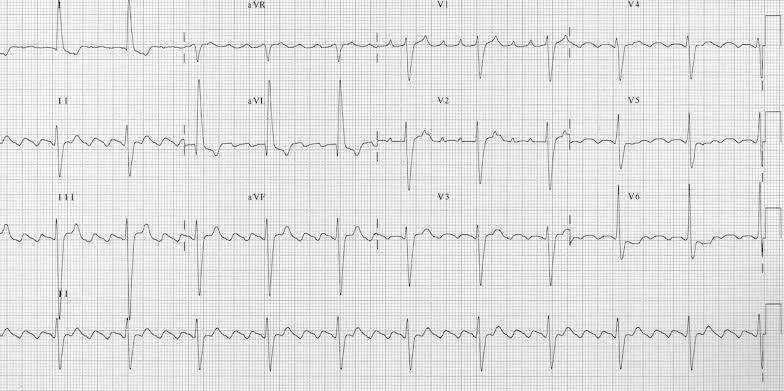
- Atrial Flutter: Electrical signals in the atria typically cycle rapidly in a specific pattern (often a “sawtooth” pattern), usually in the right atrium. This cycle causes the atria to contract very rapidly but usually in a regular rhythm (flutter). The signal transmitted to the ventricles does not occur with every atrial beat, but at specific ratios (e.g., 2:1, 3:1, or 4:1). This results in ventricular beats that are rapid but generally regular or more regular. On an EKG, characteristic “flutter” waves (F waves) are seen instead of P waves.
In short, while the atria “quiver” in AF, they “flutter” in a regular but rapid manner in atrial flutter. Both conditions carry a risk of stroke, and while their treatment approaches are similar, their mechanisms and EKG appearances differ. As a cardiologist, making this distinction correctly is vital for accurate diagnosis and treatment.
What Symptoms Does Atrial Flutter Show? Your Heart’s Signals
The symptoms of atrial flutter can vary from person to person. Some people may feel no symptoms at all, while others may experience quite distressing ones. The most common symptoms include:
- Palpitations: This is one of the most frequent symptoms. You might feel your heart beating fast, strongly, racing, or irregularly.
- Shortness of Breath: This can occur due to the heart’s inefficient pumping, leading to insufficient blood flow to the lungs or fluid buildup in the lungs. It may worsen with exertion.
- Fatigue and Weakness: Due to the body not receiving enough oxygen and nutrients, a feeling of low energy may be experienced. Difficulty performing daily activities might occur.
- Chest Pain or Discomfort: Rapid heartbeats can increase the heart’s oxygen demand, which may manifest as pressure, tightness, or pain in the chest. This can be more pronounced in individuals with coronary artery disease.
- Dizziness or Lightheadedness: This can happen if there isn’t enough blood flow to the brain.
- Fainting (Syncope): Although rare, extremely rapid heartbeats can severely reduce blood flow to the brain, leading to fainting.
- Anxiety and Apprehension: An irregular heartbeat can cause feelings of restlessness and panic in individuals.
If you experience any of these symptoms, especially if they appear suddenly or are severe, it is crucial to seek immediate medical attention from a cardiology specialist. Early diagnosis and intervention are critical to preventing possible complications.
What Are the Causes of Atrial Flutter? Triggering Factors
While the exact cause of atrial flutter cannot always be determined, it is usually associated with a structural problem in the heart or another underlying medical condition. Here are conditions that increase the risk or directly cause atrial flutter:
- Heart Diseases:
- Coronary Artery Disease (CAD): Narrowing or blockage of the arteries supplying the heart.
- Hypertension (High Blood Pressure): Long-term uncontrolled high blood pressure can lead to structural changes in the heart.
- Heart Failure: A condition where the heart cannot pump enough blood to the body.
- Heart Valve Diseases: Problems with the heart valves (narrowing or insufficiency).
- Previous Heart Surgery: Scar tissue formed in the atria, especially after heart valve or coronary bypass surgeries, can predispose to rhythm disorders.
- Congenital Heart Defects: Structural heart abnormalities present from birth.
- Lung Diseases:
- Chronic Obstructive Pulmonary Disease (COPD): Chronic inflammation and restricted airflow in the lungs can affect the heart.
- Pulmonary Embolism: Blood clots in the pulmonary arteries can put excessive strain on the heart.
- Sleep Apnea: Repeated pauses in breathing during sleep stress the heart.
- Endocrine Disorders:
- Hyperthyroidism (Overactive Thyroid Gland): High levels of thyroid hormones can cause the heart to beat rapidly and lead to arrhythmia development.
- Other Conditions:
- Obesity: Excess weight increases the risk of many heart diseases, including atrial flutter.
- Diabetes: Diabetes can lead to vascular damage and trigger heart diseases.
- Excessive Alcohol Consumption: Heart rhythm disturbances can occur after excessive alcohol intake, also known as “holiday heart syndrome.”
- Excessive Caffeine or Certain Medications: Some stimulants or medications (e.g., decongestants) can affect heart rhythm.
- Electrolyte Imbalances: Especially disturbances in the levels of minerals like potassium and magnesium.
- Sepsis or Severe Infections: The body’s general inflammatory response can affect the heart.
The combination of one or more of these causes increases the risk of developing atrial flutter. Identifying the underlying cause plays a key role in managing the disease and preventing its recurrence.
What Risks Does Atrial Flutter Pose? Potential Complications
If left untreated, atrial flutter can lead to serious health problems. The most significant risks include:
- Stroke: In atrial flutter, because the atria do not contract regularly and completely, blood flow slows down, increasing the risk of blood clots forming within the atria. These clots can break off from the heart and travel to the brain, blocking an artery and causing an ischemic stroke. Atrial flutter carries a significant risk of stroke, although it may be lower than in atrial fibrillation.
- Heart Failure: Prolonged rapid heartbeats (tachycardia) can tire the heart muscles and eventually lead to a decrease in the heart’s pumping ability, causing tachycardia-induced cardiomyopathy and heart failure. Symptoms of heart failure include shortness of breath, fatigue, and leg swelling.
- Other Cardiovascular Events: Atrial flutter can increase the risk of heart attack or sudden cardiac death, especially if there are other underlying heart conditions.
- Reduced Quality of Life: Persistent palpitations, shortness of breath, and fatigue can limit a person’s daily activities, reduce work performance, and negatively impact overall quality of life. Anxiety and depression are also common psychological effects.
Due to these risks, it is vital for individuals diagnosed with atrial flutter to receive regular follow-up and appropriate treatment.
How Is Atrial Flutter Diagnosed? Diagnostic Methods
To diagnose atrial flutter, a cardiologist uses various methods. The diagnostic process typically includes the following steps:
- Detailed Patient History and Physical Examination: The doctor will inquire about the patient’s symptoms (palpitations, shortness of breath, fatigue, etc.), when they started, their severity, and triggers. Previous medical conditions, medications used, and family history are also important. During the physical examination, heart sounds are listened to, pulse is checked, and blood pressure is measured.
- Electrocardiography (EKG): This is the most basic and rapid tool for diagnosing atrial flutter. The EKG records the heart’s electrical activity graphically on paper. The presence of characteristic “sawtooth” shaped F waves for atrial flutter and a regular atrial activity with a specific ratio of ventricular response (e.g., 2:1, 3:1) helps in diagnosis.
- Holter Monitoring: If the arrhythmia cannot be captured during an EKG (because the arrhythmia may not be continuous), a Holter monitor, a portable EKG device that continuously records heart rhythm for 24-48 hours or longer, is used. This allows for the detection of rare or intermittent atrial flutter attacks.
- Event Recorder: In some cases, if symptoms occur less frequently, event recorders that can be activated by the patient or automatically record at certain arrhythmia thresholds may be used.
- Echocardiography (Echo): This is an ultrasound examination of the heart. It provides detailed information about the heart’s structure, chamber size, valve function, and pumping strength. It is important for detecting any underlying heart conditions (valve disease, heart enlargement, etc.) that could cause atrial flutter.
- Blood Tests: Tests such as thyroid function tests (to rule out hyperthyroidism), electrolyte levels, kidney function tests, and blood sugar are checked to identify underlying causes or co-existing conditions that may contribute to atrial flutter.
- Angiography: Contrast dye is injected into the heart’s blood vessels and imaged under X-ray. It is the gold standard method for definitively identifying narrowings or blockages in the vessels.
- Cardiac MRI or CT Angiography: These are advanced imaging techniques that provide more detailed views of the heart and blood vessels. They may be preferred in cases of complex heart diseases or when angiography cannot be performed.
- Electrophysiological Study (EPS): Rarely, in patients where diagnosis is difficult or ablation therapy is planned, an invasive test called an electrophysiological study may be performed to map the electrical pathways in the heart in detail.
Through a combination of these tests, the diagnosis of atrial flutter is confirmed, and the patient’s condition is best evaluated.
Atrial Flutter Treatment Algorithm: Treatment Options
Treatment for atrial flutter is determined based on the severity of symptoms, underlying causes, the patient’s overall health, and stroke risk. The treatment algorithm typically includes the following steps:
1. Acute Attack Treatment (Rhythm Control and Rate Control):
- Rate Control: Controlling the heart rate is important. Medications such as beta-blockers (e.g., metoprolol, bisoprolol) or calcium channel blockers (e.g., diltiazem, verapamil) are used to reduce the number of atrial signals transmitted to the ventricles and bring the heart rate back to near-normal levels.
- Rhythm Control (Cardioversion): The aim is to restore normal sinus rhythm from atrial flutter.
- Pharmacological Cardioversion: Anti-arrhythmic drugs (e.g., ibutilide, flecainide, propafenone, amiodarone) are used to try and restore normal heart rhythm.
- Electrical Cardioversion: A controlled electrical shock is delivered to the chest via electrodes to help the heart return to its normal rhythm. This is preferred in emergency situations or when drug therapy is unsuccessful.
2. Reducing Stroke Risk (Anticoagulation):
Atrial flutter, like atrial fibrillation, increases the risk of blood clot formation in the atria and thus the risk of stroke. Therefore, the patient’s stroke risk is assessed using the CHA2DS2-VASc score. In high-risk patients (or those above a certain score), anticoagulant (blood-thinning) medications are initiated. These medications significantly reduce the risk of stroke by preventing clot formation. Newer oral anticoagulants (NOACs) or traditional warfarin may be used. This treatment often continues long-term, sometimes even lifelong, even if the patient’s rhythm returns to normal.
3. Long-Term Rhythm Control and Recurrence Prevention:
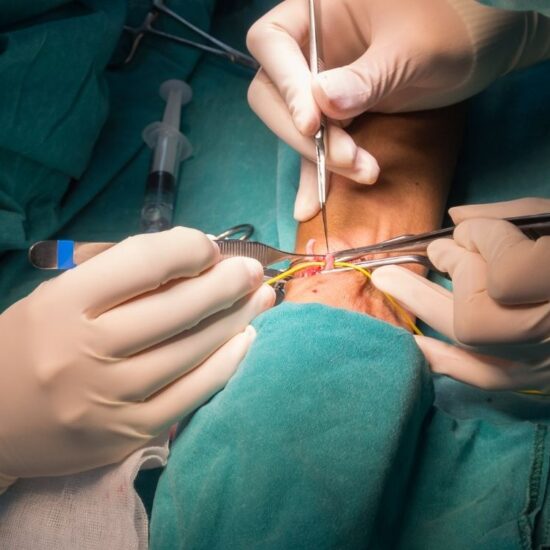
- Catheter Ablation: This is one of the most effective and often first-line treatments for atrial flutter. Through thin catheters inserted via groin veins, the heart tissue that forms the electrical circuit causing the rhythm disorder (typically the “cavotricuspid isthmus” in the right atrium) is burned or frozen using radiofrequency energy or cryotherapy. This procedure interrupts the flutter circuit, allowing the normal sinus rhythm to return, and has a high success rate.
- Anti-arrhythmic Medications: In patients after cardioversion or where ablation is not suitable, long-term anti-arrhythmic drug therapy (e.g., amiodarone, flecainide, sotalol) may be used to prevent recurrence of the rhythm. However, the side effects and effectiveness of these drugs must be carefully evaluated by the doctor.
4. Treatment of Underlying Causes:
Proper treatment of conditions that cause or increase the risk of atrial flutter, such as high blood pressure, diabetes, thyroid diseases, or heart failure, is critically important for controlling atrial flutter and preventing its recurrence. Lifestyle changes (healthy diet, exercise, weight management, quitting smoking) are also indispensable in this process.
The treatment decision should be made by a cardiologist based on the patient’s individual circumstances.
Additional Heading: Living with Atrial Flutter: Supportive Approaches
Receiving an atrial flutter diagnosis and starting treatment can be concerning for some patients. However, with the right information and supportive approaches, it is possible to cope with this condition.
- Importance of Medication Adherence: Taking your prescribed medications regularly and correctly is vital for the effectiveness of treatment and the prevention of complications. Consult your doctor if you suspect any side effects or drug interactions.
- Sustainability of Lifestyle Changes: It’s important to maintain heart-healthy lifestyle choices not just during treatment but for the rest of your life. Habits such as a healthy diet, regular exercise, weight management, and avoiding smoking and excessive alcohol will help prevent atrial flutter recurrence and improve your overall heart health.
- Stress Management: Stress can negatively affect heart rhythm. Learning to manage stress through methods like meditation, yoga, deep breathing exercises, developing hobbies, or seeking professional support can be beneficial.
- Symptom Tracking and Recording: Keeping a record of the frequency, duration, and severity of your atrial flutter symptoms (palpitations, shortness of breath, etc.) can help your doctor better understand your condition and adjust your treatment plan.
- Regular Check-ups: Attending regular follow-up appointments with your cardiologist is essential for monitoring your condition and early detection of potential complications.
- Patient Education and Awareness: Learning about atrial flutter, understanding what situations trigger it, and knowing emergency symptoms will help you feel more secure.
Frequently Asked Questions About Atrial Flutter
As a cardiologist, I frequently hear these questions about atrial flutter from my patients. Here are my answers:
1. Is atrial flutter genetic?
It is not entirely a genetic disease, but some genetic factors or hereditary heart conditions can increase the risk of atrial flutter. The risk may increase if there is a family history of heart rhythm disorders.
2. Can atrial flutter be completely cured?
High success rates can be achieved with treatments like catheter ablation, and most patients can return to normal sinus rhythm. However, recurrence may occur in some cases, or long-term medication may be required. It might be more accurate to use the term “effectively managed” rather than “completely cured.”
3. Can I exercise with atrial flutter?
Generally, once atrial flutter is controlled and your doctor approves, you can exercise. However, you may need to avoid extremely strenuous activities or adhere to specific restrictions. It’s important to discuss with your doctor to determine an appropriate exercise plan for you.
4. Do I need to take blood thinners for life?
Depending on your stroke risk, your doctor may recommend blood thinners long-term or for life. This decision is made by your doctor because the risk of clot formation can persist even if your rhythm returns to normal. Stopping these medications carries sudden and serious risks.
5. Does atrial flutter affect psychological well-being?
Yes, the symptoms caused by atrial flutter (palpitations, shortness of breath) and the anxiety it brings can lead to stress, anxiety, and even depression. Do not hesitate to seek psychological support in such cases.
6. How should caffeine and alcohol consumption be managed with atrial flutter?
Caffeine and alcohol can trigger atrial flutter attacks in some individuals. The amount consumed and individual tolerance are important. Generally, moderate consumption or complete avoidance may be recommended. It is best to consult your doctor on this matter.
Conclusion: Take Conscious Steps for Your Heart
Dear readers, atrial flutter is a heart rhythm disorder that needs to be recognized and taken seriously. However, thanks to the diagnostic and treatment methods offered by modern cardiology, it is possible to cope with this condition and lead a healthy life. If you experience any symptoms related to your heart or have concerns, do not hesitate to consult a specialist without delay. Remember, every conscious step you take for your heart is a significant step towards a healthier future.
Stay with a healthy heart!